Original studies Volume 13, No.4 • 2012
UDC: 616.728.3-001 +617.583
Buryanov O.A., Omelchenko T.M., Sobolevskyi Y.L., Skopenko Y.O.
Bohomolets National Medical University, Kyiv, Ukraine
Introduction. Juxta- and intra-articular fractures of bones belong to a spread type of lesions, suffered by people of different age groups. Their occurrence, according to literature data, reaches 25-40% [1, 10, 13, 14]. In majority of patients the modern treatment principles of such lesions – accurate reposition and early function can be ensured only by means of surgical treatment – open repositions and stable-functional osteosynthesis. Though, even under such conditions, complications occurrence rate reaches 6%-8%, and number of unsatisfactory results of treatment in general ranges from 7% to 38% [1, 4, 8, 9, 10].
An early and rapid development of post-traumatic osteoarthritis, causing primary disability of patients from 8.8% to 46%, constitute the main unsatisfactory result of intra-articular lesions treatment. Consequently, intra-articular lesions of knee and ankle joints are leading in disability structure as regards of patients with results of joints traumas [1, 10, 14].
Despite success of the modern traumatology, the problem of treating the intra-articular fractures with articular cartilage lesion can’t be considered resolved in connection with too high percent of unsatisfactory results.
The works, published by a range of native and foreign scientists, demonstrate that even upon condition of perfectly performed fragments reposition and stable-functional osteosynthesis in case of intra-articular osteochondral fractures, the occurrence of rapidly progressing degenerative changes in a joint reaches 12%-17%, that causes disability and necessity of subsequent reconstructive surgical interferences during the first years after trauma [1, 4, 5, 14]. It is determined, that an early and rapid development of a posttraumatic osteoarthritis depends on nature and articulate hyaline cartilage lesion area, as well as faults in rehabilitation and absence of appropriate treatment measures, aimed at maintenance and regeneration of an articular hyaline cartilage [1, 5, 7, 10].
Usually defects of articular cartilage practically do not regenerate, most commonly they are replaced with fibrocartilage. In case of joints traumatic lesion, metaplasia or disregeneration occur, a hyaline cartilage is replaced with a low-constancy fibrocartilage and a weak contact with a subchondral bone plate. As a rule, lesions around synovial membrane heal due to low-differentiated cells of connective tissue. They can be filled with fibrocartilage. It is determined, that chondrocytes do not migrate from the defect-adhering articular cartilage segments to the defect area [2, 3].
Buryanov O. A et al. have experimentally proven that in case of intra-articular traumatic lesions enormous local acceleration of free radical peroxidation occurs, being the key pathogenetic mechanism in osteoarthritis development that is often left without treatment. Besides, a trauma is accompanied by hemarthrosis and inflammation, accelerating destruction of a cartilage and initiating chondrocyte apoptosis [3, 6, 7, 11].
A range of experimental clinical researches with implementation of morph-histological methods ascertains the possibility of directed correction of cartilage reparation with the use of developed complex of pharmacological treatment with drugs of chodro-modificating and anti-oxidant action (Buryanov O.A. et al., 2007, 2009, 2010). The mentioned studies have shown that in case of fresh transchondral lesion of an articular cartilage, provided the maintenance or restoration of articular surface congruence and articulation biomechanical axle, the pharmacological correction contributes to formation of cartilaginous regeneration in bone-cartilagous defect, being by its histological structure close to a hyaline cartilage.
Application of the developed complex in case of old lesions is accompanied by formation of fibrous and fibrous-bone regeneration (Buryanov O.A., Brusko A.T., Omelchenko T.M., Sobolevskyi Y.L., 2008).
Moreover, it is proved that formation of the cartilagous regeneration, similar in structure to the hyaline cartilage, occurs only under conditions of transchondral lesion, because stem cells elements of subchondral bone marrow constitute the source of reparative process (Buryanov O.A. et al., 2008) [2, 3, 7].
The developed method of medicinal treatment optimizes conditions for differentiation of polyblast cells into chondroblast and chondrocyte and amplifies their metabolic activity with creation of cartilagous regeneration, similar in structure to the hyaline cartilage. Insertion of pharmacological remedy directly to the seat of a pathological process ensures rapid achievement of a clinical effect and causes formation of a necessary medium for differentiation of chondroid row cell elements, their trophism and metabolic activity [7].
Taking into consideration the above mentioned, the use of a combined drug of chondroprotective and anti-oxidant actions “Diart”, able to directly impact an articular cartilage lesion zone, it is a pathogenetically reasonable method of osteoarthritis prevention and treatment in case of intra-articular fractures.
Effective combination of hyaluronic acid and sodium succinate in drug “Diart” ensures its unique impact on articular cartilage metabolism in case of osteoarthritis and other cartilage lesions. Hyaluronic acid, that can be found in “Diart”, normalizes viscous-elastic, amortizing and greasing properties of joint fluid, impacts the nociceptors of synovial membrane intermediate layer and decreases pain mediator induction, forms a base for aggrecan, important for ensuring articular cartilage structural and functional integrity, retains water molecule to provide the joint fluid with necessary physical properties, exerts protective effect as regards of cartilaginous tissue cells – chondrocytes.
Additionally, exogenic hyaluronic acid stimulates endogenous hyaluronic acid synthesis and cartilage extracellular matrix components synthesis, decreases the level of chondrocytes apoptosis [7, 16, 17].
At this, sodium succinate in “Diart” ensures normalization of intracellular metabolism and tissue respiration under conditions of hypoxia, restoring NAD+ (nicotine amide adenine dinucleotide) through back electron transfer mechanism in mitochondrion respiratory chain, takes part in monooxygenase system of endoplasmic reticulum xenobiotic biotransformation, normalizes physiological condition and a range of indexes of acid-alkali balance in case of acidosis due to change of hydrogen ions beyond mitochondria, takes part in K+ and Ca2+ transportation control, ensures stabilization of oxidative and anti-oxidative balance, reduces reaction intensity of lipids free radical peroxidation [12].
Purpose of the research. Assessing the efficiency of using the hyaluronic acid and sodium succinate (“Diart”) combined drug for prevention of post-traumatic osteoarthritis development during treatment of intra-articular fractures with articular cartilage lesion.
Study material and methods. Complex therapy and examination was held in 86 patients that were treated in connection with close intra-articular fractures of shin bone proximal epimetaphys with displacement. All patients underwent surgical interference – open fragment reposition and stable-functional osteosynthesis. Patients’ average age was 37±5.8 years. The number of male patients amounted to 36 (60%), female patients made – 24 (40%). Lesion type was determined according to AO classification. Patients with intra-articular lesions of moderate severability composed observation groups. According to AO/А5ІР classification the patients with lesions of В1, В2, С1 and С2 (Fig.1) types were chosen among shin bone proximal epimetaphys lesions. Patients’ division into observation groups is shown in Table 1. The main patients group comprised 44 patients, comparison group comprised 42 patients.
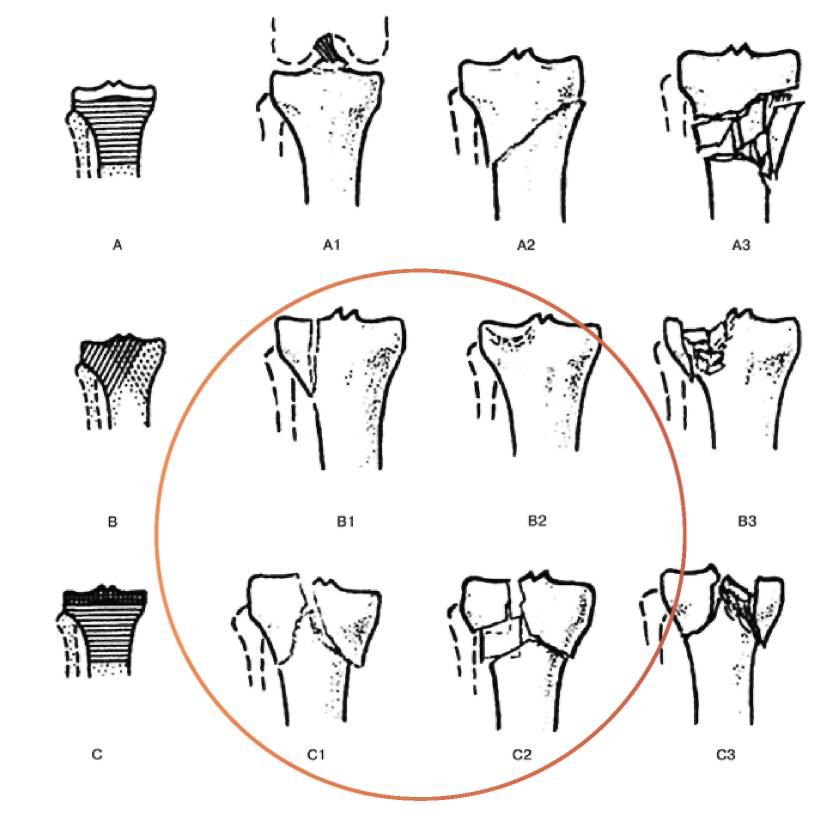
Figure 1. Shin bone proximal part fracture classification according to АО/АSІF classification, showing types of fractures, included into the study.
Table 1
Patients’ division in observation groups, depending on trauma type according to АО/АSІF classification (n1=44; n2=42)
| Lesion nature | Knee joint intra-articular fractures (shin bone proximal epimetaphys) | |||||||||
|
Trauma type according to АO/АSІF |
B1 | B2 | C1 | C2 | Total number in group | |||||
| Patients number | n | % | n | % | n | % | n | % | n | % |
| Main group n1=44 | 18 | 21% | 12 | 14% | 9 | 10% | 5 | 6% | 44 | 51% |
| Comparison group
n2=42 |
17 | 20% | 14 | 16% | 7 | 8% | 4 | 5% | 42 | 49% |
| Total | 35 | 41% | 26 | 30% | 16 | 18% | 9 | 11% | 86 | 100% |
Surgical treatment. Surgical interference was performed in both groups after a pre-operation examination and preparation complex – open fragment reposition and stable-functional osteosynthesis according to classical method with the use of metal osteosynthesis technique, depending on trauma type. Reposition accuracy in all patients was arthroscopically controlled. In all cases including accompanying lesions of articular cartilage, the abrasive plastics and high-frequency modification was resorted to; in case of meniscus lesions they were maintained to the possible extent (minimal resection of destroyed parts, meniscus suture, needling, etc.), in case of crucial ligament lesion with bone fragment available, refixation of bone bed was performed; if bone fragment was absent, ligament residual limb was arthroscopically operated, and the issue of its restoration was carried over to the other stage (after bone union and movement recovery in a joint, provided that a knee joint was unstable).
Post-operation treatment and rehabilitation
|
During the first week after surgery |
|
Calmness, knee joint immobilization with a frame, isometric contraction of thigh and crus muscles (remedial gymnastics within the I period) |
| In 5-7 days after surgery (provided the complete stabilization of patient’s status, drain removal, normal primary healing of post-operation wounds without signs of inflammation) |  |
Passive movements in a knee joint (remedial gymnastics within the II period) with gradual amplitude increase during 2 weeks |
|
3.5 – 4 weeks after operation (in 1.5 – 2 weeks after sutures removal) |
 |
Active movement development, remedial gymnastics within the III period, massage, phonophoresis with non-steroidal anti-inflammatory drugs and chondroprotectors |
|
Within 2 – 3 months after surgery |
 |
Active movements without load (without load on the operated extremity), depending on fracture type |
|
Since the first week after surgical interference |
 |
Non-steroidal anti-inflammatory drugs, antioxidants, chondroprotectors, complex calcium drugs with vitamin D3 |
|
After full vanishing of all inflammation symptoms and absence of exudate in a joint (in 5-6 weeks after operation) |
 |
Intra-articular injection therapy with hyaluronic acid and sodium succinate combined drug “DIART” |
During the first week after operation the patients are prescribed calmness, knee joint immobilization with a frame, isometric contraction of thigh and crus muscles (remedial gymnastics within the І period). In 5 – 7 days after surgical interference (provided the complete stabilization of patient’s general status, drain removal, normal primary heal of post-operation wounds without signs of inflammation) – passive movements in a knee joint were prescribed (remedial gymnastics within the ІІ period) with gradual amplitude increase during 2 weeks.
In 1.5-2 weeks after sutures removal (corresponding to 3.5 – 4 weeks after operation) active movement development, remedial gymnastics within the III period, massage, phonophoresis with non-steroidal anti-inflammatory drugs and chondroprotectors were prescribed. Considering the availability of metal fixation, other physiotherapeutic procedures (ultrahigh frequency therapy, magnet, thermal procedures, electrophoresis, etc.) were not categorically conducted for patients. Active movements without load (without load on the operated extremity) were prescribed during 2-3 months after operation, depending on fracture type. During the first week after surgical interference a complex of medicinal treatment was prescribed in both clinical groups, aimed at weakening of posttraumatic inflammatory process, stabilization of oxidative and anti-oxidative balance, activation of cells metabolism of chondroid range, optimization of reparative osteogenesis.
In such a way, a general non-steroidal anti-inflammatory drugs course lasting for 10-14 days was prescribed in a comparison group (n2=42) , antioxidants were prescribed for 30 days, chondroprotectors (chondroitin and glucosamine sulphate) were prescribed for 60 days, and complex calcium drugs with vitamin D3. All medicinal drugs were prescribed in generally recommended dozes, considering individual features, age and accompanying patients’ pathology.
A course of intra-articular injection therapy with a hyaluronic acid and sodium succinate combined drug “Diart” 1.1% 2.0 ml No. 3 was carried out in the main patients group (n1=44), apart from the identical medicinal treatment course. Intra-articular injection of “Diart” was performed after full vanishing of all inflammatory symptoms with absence of exudate in a joint that was seen in average in 5-6 weeks after operation and determined according to clinical and ultrasonic examination data. Injection was carried out under ultrasonographic control with a 7-10 days interval.
Clinical, ultrasonographic, roentgenologic examination methods, as well as computerized tomography were used in the study. In order to assess treatment results, patients’ observation of both clinical groups was performed over time: in 3, 6 and 12 months after operation. During clinical scoring of treatment result the scoring of pain syndrome on visual analogue scale (VAS), scoring of knee joint functional condition by counting points on Lysholm scale, scoring of patients’ activity on Tegner activity level scale was used. On the basis of roentgenologic examination the X-ray signs of existence and progression of osteoarthritis was determined.
Visual analog pain scale ((VAS) of Huskisson) is a common tool of scoring the pain syndrome level in many pathological states [7]. It is a horizontal line with marks from 0 to 100 mm, the beginning of which corresponds to absence of pain sense and its end corresponds to maximal pain level. The patient is proposed to mark a point on a scale to answer the question about level of his/her pain sense.
The Lysholm knee joint functional state scoring scale based on points scoring was proposed by Lysholm and Gillquist in 1982 [7]. It is designed for filling in by a patient with doctor’s assistance. At general points scoring the result is classified as “unsatisfactory”, “satisfactory”, “good”, or “excellent”. Index 100 corresponds to an absolutely healthy knee joint. Index of 84 points is considered the lowest limit of excellent/good results.
The Tegner Activity Level scale is represented in a form of questions that examine 11 levels of patient’s possible activity. The patient is proposed to choose the activity level on his/her own, coinciding with his/her possibilities at the moment of examination. At this, 0 corresponds to maximum disorder, level 10 corresponds to full functional possibilities of a knee joint [7].
Roentgenologic examination was carried out for all patients before the start of treatment, as well as during post-operation period in 3.6 and 12 months, respectively. Roentgenograms were executed in a load in standard and, if necessary, in additional projections. Occurrence of bone union, changes of bone tissue density, presence and prevalence of regional osteophytes, symmetry and stricture level of a joint slot, intensity of degenerative-dystrophic changes in a joint (osteoarthritis stage according to Kellgren&Lawrence) were assessed on roentgenograms.
Research results and their discussion. Functional result was the better, the less intensive was pain syndrome on VAS, the more the sum of points on Lysholm scale approached 100, the higher activity level was observed on Tegner scale (the more its index was close to 10). Roentgenologically the treatment results were the better, the less signs of a degenerative-dystrophic process were found in a knee joint. The general score of the treatment results is shown in Table 2.
General clinical score of treatment results (М±m) (n1=44; n2=42)
| Observation groups | ||||||||
| Scoring parameters | In 3 months | In 6 months | In 12 months | |||||
| Main n1 | Comparison n2 | Main n1 | Comparison n2 | Main n1 | Comparison n2 | |||
| Visual – analogue pain scale, Huskinsson | 54,7 ± 2,4 | 71,2 ± 1,5** | 7,3 ± 1,7** | 23,4 ± 1,6** | 10,1 ± 1,6** | 17,3 ± 0,6* | ||
| Average index on Lysholm scale (in points) | 45,8 ± 2,7 | 32,6 ± 2,9* | 84,7 ± 3,1** | 69,8 ± 3,6** | 95,6 ± 1,2 | 72,6 ± 2,4** | ||
| Scoring on Lysholm scale (patients, %) | Excellent | – | – | 21,3 | 8,9 | 34,3 | 21,9 | |
| Good** | 42,3 | 27,9 | 60,8 | 46,3 | 59,7 | 56,8 | ||
| Satisfactory** | 57,7 | 68,3 | 17,9 | 44,8 | 6,0 | 21,3 | ||
| Unsatisfactory** | – | 3,8 | – | – | – | – | ||
| Tegner Activity Level scale (in points) | 5,8±0,2 | 3,1 ±0,8 | 7,6 ± 1,5** | 5,3 ± 1,8** | 9,3 ± 1,6** | 7,2 ± 1,7** | ||
|
Intensity of post-traumatic degenerative changes in a joint (OA stage according to Kellgren&Lawrence), patients, % |
0 | 10,3±0,8 | 2,8±2,1** | 9,6±0,7 | 1,2±0,4** | 9,5±1,1** | – | |
| I | 79,7±0,4 | 86,4±0,9* | 79,2±1,4 | 75,1±1,5* | 80,2±1,8* | 74,8±1,9* | ||
| II | 10,0±1,3 | 10,8±0,4 | 11,2±1,7 | 15,3±0,9* | 10,3±08 | 12,9±1,2* | ||
| III | – | – | – | 8,4±0,2* | – | 12,3±0,8* | ||
| IV | – | – | – | – | – | – | ||
Note: * – р < 0.05;** – р < 0.01 when comparing in groups in dynamics.
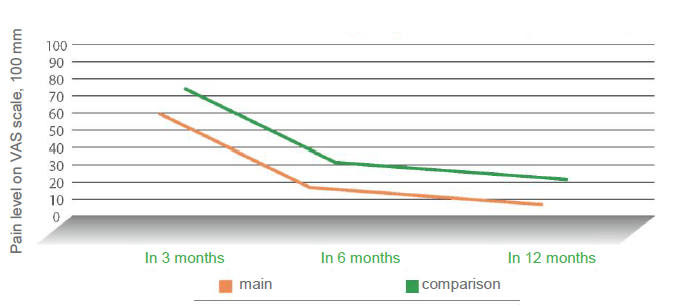
Pain syndrome intensity on VAS (VAS, Huskisson)
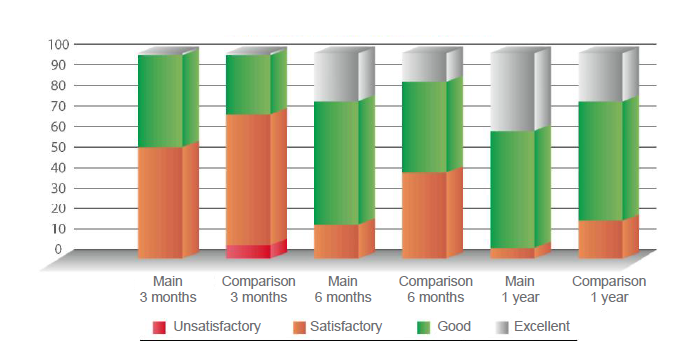
Scoring on LYSHOLM scale
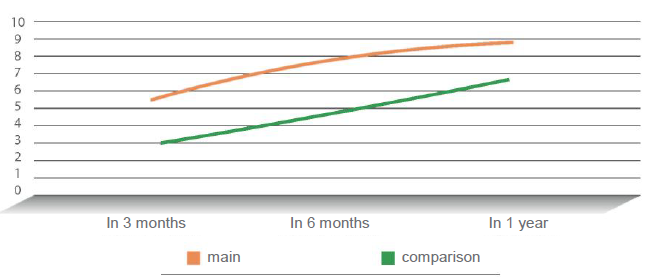
Activity level in TEGNER scale
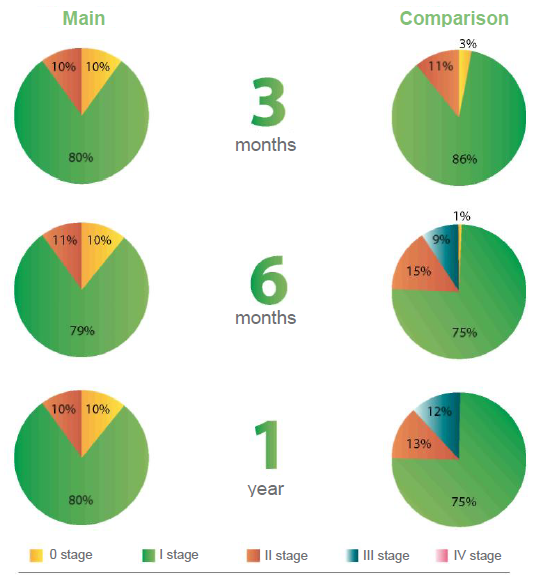
Dynamics of post-traumatic degenerative-dystrophic changes in a traumatized joint in patients of the main and comparison groups
Analysis of pain syndrome dynamics in patients of the main and comparison groups on visual analogue scale VAS showed that in 3 months after operation the average pain index amounted to 54.7 ± 2.4 in patients of the main group, undergoing five-fold course of intra-articluar treatment with “Diart” drug, if compared to 71.2 ± 1.5 in patients of the comparison group, being almost 1.5 times more.
In 6 months after treatment a considerable decrease of pain syndrome was detected in both groups. This fact was connected with receipt of full course of medicinal treatment and rehabilitation, patients’ activation, possibility of full loading and maximal restoration of active movements in a joint. At that, pain syndrome was 17.3 in the main group and 23.4 in the comparison group. Apparently, irrespective of general pain syndrome intensity decreasing, the pain level in the main patients group, as before, was 1.5 times lower than in the comparison group. Similar dynamics was detected in 12 months (Table 2).
Knee joint functional state scoring to LYSHOLM scale trustworthily showed better functional result in the main group. At this, excellent results were detected during 6 months period, being 2.5 times bigger in the main group, in which the combination of hyaluronate and succinate was used, in contrast to the comparison group (21.3% and 8.9%, respectively). A trustworthy rapid rate of positive increase of a knee joint function is detected in observation dynamics in patients of the main group on the Lysholm scale. In 12 months, functional activity index of the main group patients reached 95.6 with 94% of excellent and good results. The respective index in the comparison group was 72.6 in 1 year, and the per cent of excellent and good results amounted to only 79.7% (Table 2).
Determination of patients’ activity on the TEGNER scale ascertained: activity level of patients, receiving in a complex of medicinal treatment intra-articular hyaluronate and succinate in “Diart” during 3-months period, was almost 6 point – that is twice bigger than in comparison group patients. Activity increase during 6- and 12-months observation period was noticed in both groups, but its rate was greater in the main group, and at the end of the research the average rate in the main group reached 9.3 points. At the very same time in comparison group average rate amounted to 7.2, corresponding to 6-months index of the main group (Table 2).
Post-traumatic degenerative changes intensity in a joint was determined finding out the stage of osteoarthritis according to Kellgren & Lawrence classification on the basis of standard roentgenologic symptoms occurrence: stricture level of a joint slot, its asymmetry, assessment of level and prevalence of subchondral osteosclerosis, presence and prevalence of regional osteophytes, joint deformation, etc.
It was determined that, despite the performed treatment, the traumatic lesion of the articular cartilage always caused development of degenerative changes in it, and the grade of their intensity is determined by lesion severity. This being the case, signs of osteoarthritis of the first stage, already in three months after trauma, were found in 79% of patients in the main patients group, in 10% signs of the second stage were found, and only 11% of patients didn’t have osteoarthritis signs. At the same time, signs of osteoarthritis were absent only in 2.8% of patients of the comparison group, first stage was detected in 86% and second stage was detected in 11%. Though, in observation dynamics it was found out that progressing of post-traumatic changes in a knee joint was insignificant in patients of the main group. In 12 months patients’ distribution was left practically without changes. A negative dynamics and significant progressing of degenerative-dystrophic changes in a joint was detected in the comparison group. At that, in six months osteoarthritis of the first stage was detected in 75% of patients, per cent of patients with the second stage raised up to 15%, and 8.5% of patients with the third stage of post-traumatic gonarthrosis appeared. For 12 months, insignificant, but negative further redistribution occurred in this group, accompanied by increase of patients with gonarthrosis up to 12.5% (Table 2).
Conclusions. It is defined that traumatic lesion of an articular cartilage always initiates degenerative-dystrophic changes in it and causes development and rapid progressing of osteoarthritis that makes actual early usage of both general and local measures on articular hyaline cartilage maintenance, as well as stimulation and optimization of its reparation.
Study results of a pain syndrome, level of functional capability of a knee joint and patients’ activity in the main and comparison clinical groups have reliably shown advantage of “Diart” usage in the aspect of efficiency and dynamics of pain syndrome decrease, rate of movement activity restoration and stability of treatment results.
Absence of negative dynamics of post-traumatic degenerative-dystrophic changes progression in a disordered joint in the main clinical group testified to efficiency of hyaluronate and succinate combination in “Diart” in the aspect of anabolism enhancement in a disordered articular hyaline cartilage, stimulation and optimization of its reparation.
Literature is under consideration
